On 21 September 2022, NCITA hosted the fifth lecture in the NCITA ‘On the Shoulders of Giants’ educational lecture series: ‘Talking with patients about sad, bad and just plain difficult things’ with Professor Dame Lesley Fallowfield, Professor of Psycho-oncology at the University of Sussex.
Clinical trials have become increasingly complex to explain to cancer patients, and the importance of clear and effective communication between healthcare professionals and patients in this area is vital. In this lecture, Professor Fallowfield covers her fascinating career, and discusses how her research contributions in psycho-oncology have enabled the measurement of quality of life through clinical treatment trials. She explains how this has helped patients, and challenges us to consider how we can improve communications with patients throughout cancer research, clinical trials and treatment.
To watch a recording of the event please visit the NCITA YouTube channel.
Cancer is complex
Whilst we have seen huge advances in cancer understanding, diagnosis, treatment and survival, cancer is no longer simple to explain to patients.
Good communication around the topic of cancer is crucial between healthcare professionals and patients, especially as there are many sad, bad and just plain difficult areas to address. Clinical trials and randomisation in particular are complex topics to effectively communicate with patients.
“Many of our patients not only survive for longer, but also many of them survive with a better quality of life; but the downside is that cancer and its treatment is no longer simple to explain, and patients who are already experiencing emotional turmoil enter this very strange new world with esoteric language and concepts”
Professor Dame Lesley Fallowfield
Mastectomy versus breast conservation: the trial that everyone needed but nobody wanted
Working with Professor Michael Baum, in 1984 Professor Fallowfield was involved in a trial to establish the safety of breast conservation in breast cancer patients, and also measure psychological morbidity in patients who received mastectomy versus breast conservation. At the time, the terms ‘psycho-oncology’ and ‘quality of life’ were rarely used in talks, papers or trials. A small psychosocial study was completed and published in the BMJ which determined no difference between groups in both psychological morbidity and sexual activity. This challenged the assumption that women, if given the choice, would always opt for breast conservation alongside psychosocial benefits.
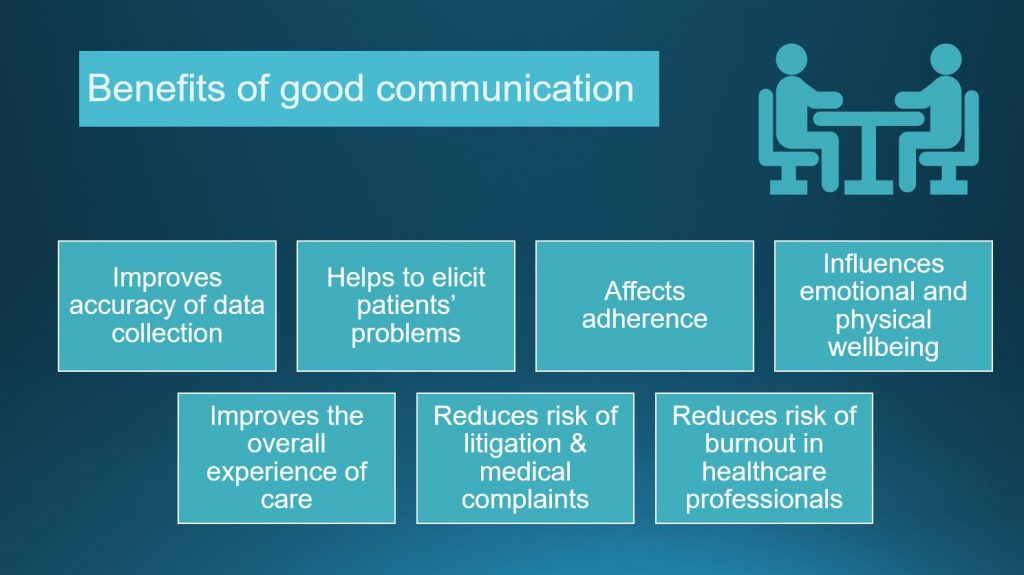
These findings led to the Choice study which assessed outside a clinical trial the psychological outcome of different treatment policies in women with early breast cancer who underwent either mastectomy or breast conservation surgery depending on the surgeon’s opinion or the patient’s choice. The results, published in the BMJ, found no significant differences in psychological morbidity either between treatments, or between those who had a real choice and those who could not chose their treatment. However, they found that women who had satisfactorily received clear and accurate information from choice surgeons, who were generally perceived to be better communicators, were less likely to be anxious and/or depressed at 12, 24 and 36 months. The Choice study therefore clearly demonstrated the importance of good communication between healthcare professionals and patients.
The complexities of explaining randomized clinical trials to patients
Alongside Professor Robert Souhami, Professor Fallowfield and her team also looked to identify and better understand the issues around the information patients received on randomized clinical trials (RCTs).
The results were interesting: whilst the majority of cancer patients were not averse to taking part in medical research, the patients found the idea of randomisation off-putting; however, when given further information about randomised clinical trials, two thirds changed their minds and consequently the majority of cancer patients had positive attitudes towards RCTs.
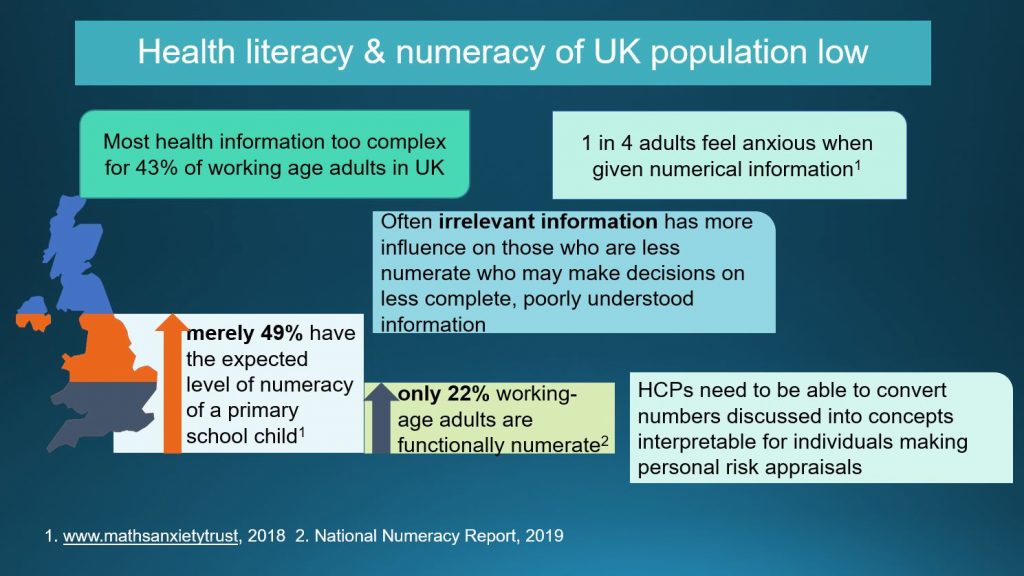
Professor Fallowfield highlighted the importance of consistent verbal and written communication. She noted that healthcare professionals cannot rely on information provided in the patient information leaflet, as it is likely to be too complex for a significant proportion of adults in the UK to fully comprehend the information provided.
“Sometimes people say to me, ‘well it doesn’t matter if I don’t tell patients about everything because they’ll read the patient information leaflet’, but many of these – even if they’re written with the help of patient advocates – are still written at far too high a literacy level. It’s a rather shocking thing to realize how low the health literacy and numeracy of UK populations are; most health information is far too complex for 43% of working age adults in the UK”
Professor Dame Lesley Fallowfield
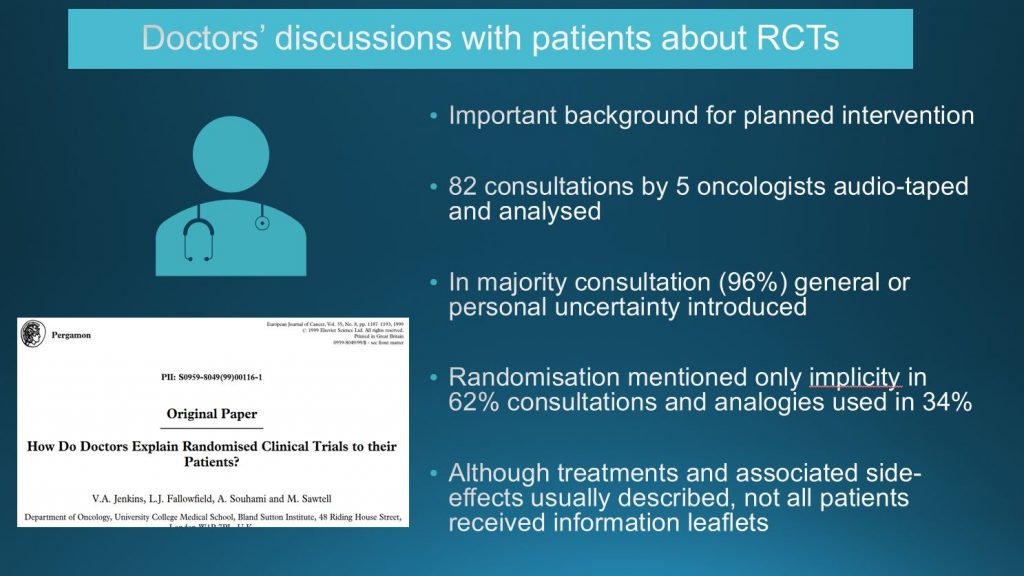
As part of a larger study designed to improve communication about randomised clinical trials (RCTs) between doctors and patients, the team audio-taped and analysed discussions between doctors and patients in which consent was being obtained for a RCT. Published in the European Journal of Cancer, the study highlighted a clear need to provide educational resources for doctors, to ensure their patients are truly able to make a clear and informed choice.
The development of an educational training programme
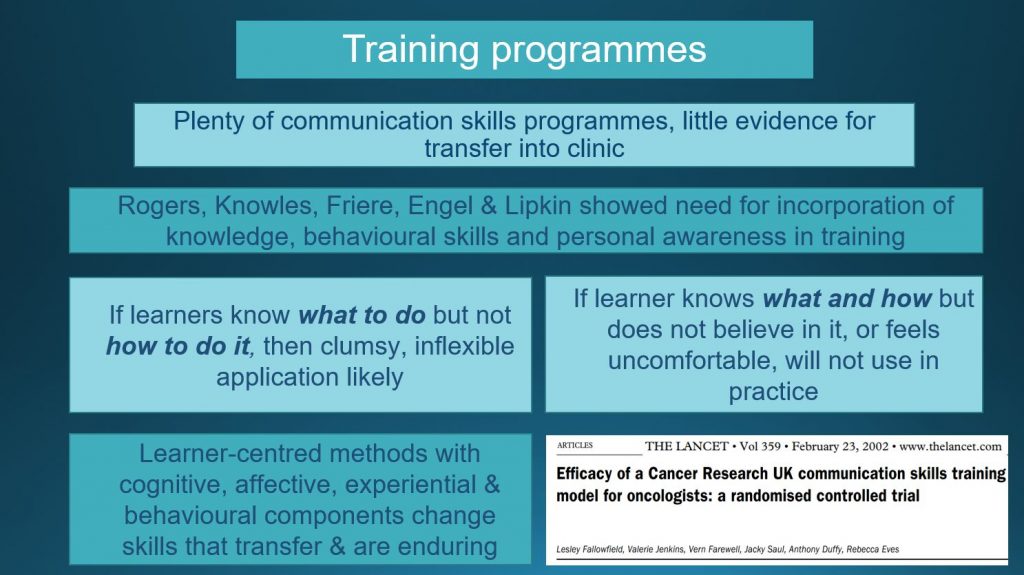
Whilst there are plenty of communication skills programmes available for healthcare professionals, there is little evidence that skills learned during the programmes transfer into clinic. Professor Fallowfield and her team carried out a randomised controlled trial in different communication skills models, and in a pivotal paper published in The Lancet they demonstrated that learner-centred methods that contain cognitive, affective, experiential and behavioural components do change skills that transfer into the clinic.
“If learners know what to do, but not how to do it, then they’re going to apply things in a clumsy and inflexible way; and if a learner knows what and how to do it but sort of doesn’t really believe in it or feels uncomfortable, they’re not going to use it in practice either. So learner-centred methods with cognitive, affective, experiential and behavioural components do change skills”
Professor Dame Lesley Fallowfield
These findings led to the development & evaluation of a training intervention aimed at improving healthcare professionals’ communication with cancer patients about randomised clinical trials. The results, published in the BMJ, demonstrated that the educational training programme significantly improved participants’ confidence and competence when communicating about randomised clinical trials.
Since that evaluation, the training programme has been adopted for training across the UK, Canada and Germany, over 200 facilitators worldwide have been trained and thousands of healthcare professionals have taken part in the training programme.
About the speaker
Dame Lesley Fallowfield is Professor of Psycho-oncology at Brighton & Sussex Medical School, University of Sussex where she is Director of the Sussex Health Outcomes Research & Education in Cancer (SHORE-C) group. Dame Lesley Fallowfield originally trained as a nurse at Guy’s Hospital, London but then did a BSc in Experimental Psychology at Sussex. Research for her doctorate examining the perceptual correlates of optic nerve damage in demyelinating diseases was completed at the Universities of Sussex and Cambridge. In 1991 she became the full-time Director of a Psychosocial Oncology Group and was awarded the first European Chair in Psycho-oncology from University College, London in 1997. Her research interests are wide and include the measurement of quality of life in clinical trials of cancer therapy and the training of communication skills for health care professionals in cancer. She has published over 400 papers, many book chapters and 3 text books. She lectures and runs training workshops throughout the world in psychosocial oncology, quality of life assessment and communication skills. She is a Fellow of the UK Academy of Medical Sciences and was made a Dame Commander of the Order of the British Empire in 2016.
About the ‘On the Shoulders of Giants’ lecture series
‘On the Shoulders of Giants’ is a series of educational talks where experts bring their perspectives to encourage and challenge wider thinking within the cancer imaging research community. See below for other lectures in the series:
- April 2022: ‘Screening for Cancer: The Good, The Bad and The Ugly’ with Prof. Michael Baum. Link to blog & recording here.
- May 2022: ‘Is Pursuing ‘a Passion for Science’ a Position of Privilege?’ with Dr Heather Williams MBE. Link to blog & recording here.
- June 2022: ‘Academia & Industry: What are the Ingredients for Successful Collaborations?’ with Kieran Murphy and Prof. Evis Sala. Link to blog & recording here.
- July 2022: ‘Striving for Evidence – With and Without a Randomised Controlled Trial’ with Professor Tom Treasure. Link to blog & recording here


